Tinea pedis is a fungal infection that affects the feet. It can also involve the interdigital spaces and the sides of the feet. The condition can present as a recurring chronic condition. Mainly caused by anthropophiles including Trichophyton rubrum, Trichophyton interdigitale, and Epidermophyton floccosum.
Question 1
Management of Tinea pedis includes both systemic and topical antifungal therapies. A period of two to four weeks is necessary for treatment with topical antifungals. They include azoles such as clotrimazole and efinaconazole, allylamines, butenafine, ciclopirox, tolnaftate, and amorolfine. Conditions such as interdigital tinea pedis may only require one week of therapy. Treatment with terbinafine or naftifine produces higher cure rates than azoles (Sahoo & Mahajan, 2016). Oral antifungal medication for tinea pedis includes terbinafine and itraconazole. Griseofulvin and fluconazole are useful for long-term treatment. Oral antifungals have been found to be more effective than topical therapy for management of tinea pedis.
Question 2
Topical ciclopirox has both antidermatophytic, antibacterial and anticandidal effects (Polat et al., 2017). The actions are important since the patient also has a history of Diabetes type 2 indicating possible immunosuppression. It works by inhibiting enzymes responsible for degrading peroxides within the fungal cell thus causing death.
Terbinafine is the most appropriate oral drug because of its safety in diabetic patients since it does not interact with the oral hypoglycemic agents that could be of use in a diabetic patient (Ilkit & Durdu, 2015). Terbinafine works by inhibiting fungal cell wall synthesis and subsequently causing fungal death.
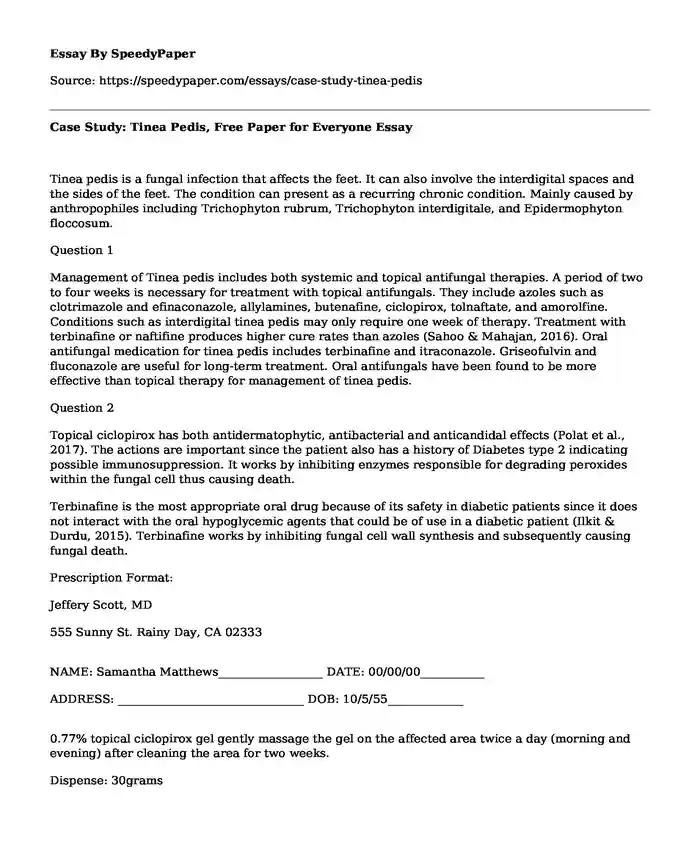
Prescription Format:
Jeffery Scott, MD
555 Sunny St. Rainy Day, CA 02333
NAME: Samantha Matthews__________________ DATE: 00/00/00___________
ADDRESS: ________________________________ DOB: 10/5/55_____________
0.77% topical ciclopirox gel gently massage the gel on the affected area twice a day (morning and evening) after cleaning the area for two weeks.
Dispense: 30grams
Refills: __1____
SIGNATURE OF PRESCRIBING PRACTITIONER: Jeffery Scott MD
NPI Number___________________________
Prescription Format:
Jeffery Scott, MD
555 Sunny St. Rainy Day, CA 02333
NAME: Samantha Matthews__________________ DATE: 00/00/00___________
ADDRESS: ________________________________ DOB: 10/5/55_____________
Terbinafine(Lamisil) 250mg Take 1 tabs once a day for 4 weeks.
Dispense: 28 tabs
Refills: __2__becasue a package has 14 tablets.
SIGNATURE OF PRESCRIBING PRACTITIONER: Jeffery Scott MD
NPI Number___________________________
Question 3.
Baseline laboratory tests before treatment will include direct microscopic examination with potassium hydroxide(KOH) preparations, a fungal culture of skin scrapings, histopathological examination with periodic acid Schiff (PAF) and use of molecular technology (Ilkit & Durdu, 2015). Antifungal susceptibility testing is also vital before initiating treatment. During treatment, necessary tests will include fungal culture, molecular methods, and microscopic examination. They are needed to monitor response to treatment. After medication, useful tests will consist of fungal culture, histopathological examination, and molecular diagnosis. They are used to test whether the treatment eradicated the fungi or was not responsive.
In KOH examination, lesions should first be cleaned with 70% alcohol to remove any skin materials or foreign products. A blunt scalpel should then be used to make the skin scrapings. The scraped cellular skin material on a microscopic slide with 15% KOH solution added is observed under a microscope after thirty minutes. Observation of septate hyphae and spores is key in making a conclusive diagnosis. A positive result gives the go-ahead to start treatment. To facilitate quick identification of hyphae and spores, blue ink, chlorazol black and rapid contrast stains may be added. The dermatophyte test strips to diagnose tinea pedis is also of importance.
Negative microscopic results do not entirely rule out the presence of the fungus and therefore essential to do a fungal culture. Although a fungal culture is inexpensive, it's time-consuming and can require two weeks to give results. Saboraud dextrose agar is the environment of choice for culture. It contains 4% peptone, 1% glucose, agar, and water. In histopathological diagnosis, three changes associated with dermatophyte infections include the presence of neutrophils, compact orthokeratosis, and appearance of the sandwich sign.
For molecular methods, nested PCR is a rapid, simple and inexpensive method for detection of dermatophytes. Diagnosis is within 48 hours. Real-time PCR is also useful for dermatophytes identification (Tsunemi et al., 2015). Antifungal susceptibility testing includes the microdilution method and determination of the minimum fungicidal concentration (MFC). MFC is the lowest drug concentration levels at which no visible fungal growth takes place.
Question 4.
After therapy, the patient can be referred in the case of non-responsiveness to medication and in the event where they develop severe tinea Pedis complications. Possible complications of tinea Pedis include cellulitis, Id reaction, majocchis granuloma, asthma, and atopic diseases. Cellulitis develops because the lesions form an entry point for bacteria. In most patients, gram-negative bacteria such as Pseudomonas, and Proteus are responsible for the cellulitis. An Id reaction is an immunological reaction. The infection may activate circulating antibodies and T lymphocytes causing generalized inflammatory responses. Patients may develop papules or pustules at secondary sites such as the fingers. In majocchis granuloma, the dermatophytes invade hair follicles causing granulomatous inflammation. Tinea Pedis infection may induce a T helper two response causing atopy. It may, therefore, complicate allergies and asthma and also cause refractory atopic disease. Superficial fungal infections can also trigger atopic dermatitis.
References
Ilkit, M., & Durdu, M. (2015). Tinea pedis: the etiology and global epidemiology of a common fungal infection. Critical reviews in microbiology, 41(3), 374-388.
Polat, A. K., Belli, A. A., Alatas, E. T., & Dogan, G. (2017). Comparison of Efficacy and Safety of Topical 1% Butenafine and Topical 1% Ciclopirox Olamine in the Treatment of Tinea Pedis and Evaluation of the Effects on the Quality of Life of These Treatmens: A Randomized Single-Blind Trial. Turk Dermatoloji Dergisi, 11(4), 174.
Sahoo, A. K., & Mahajan, R. (2016). Management of tinea corporis, tinea cruris, and tinea pedis: A comprehensive review. Indian dermatology online journal, 7(2), 77.
Tsunemi, Y., Takehara, K., Miura, Y., Nakagami, G., Sanada, H., & Kawashima, M. (2015). Diagnosis of tinea pedis by the D ermatophyte T est S trip. British Journal of Dermatology, 173(5), 1323-1324.
Cite this page
Case Study: Tinea Pedis, Free Paper for Everyone. (2022, Sep 08). Retrieved from https://speedypaper.com/essays/case-study-tinea-pedis
Request Removal
If you are the original author of this essay and no longer wish to have it published on the SpeedyPaper website, please click below to request its removal:
- Mixed Methodology - Free Paper with a Project Proposal Example
- Quality Assurance Audit Research Paper Sample
- Article Review Example: Disruptive Technology Innovation
- Leadership of Richard Branson - Essay Sample
- Free Essay: Exposure Routes and Health Effects of Heavy Metals on Children
- The Greek Financial Crisis, Essay Example
- Essay Example on Issues in Society Arose Due the Internet and Social Media
Popular categories