| Type of paper: | Essay |
| Categories: | Psychology Medicine Mental health |
| Pages: | 6 |
| Wordcount: | 1529 words |
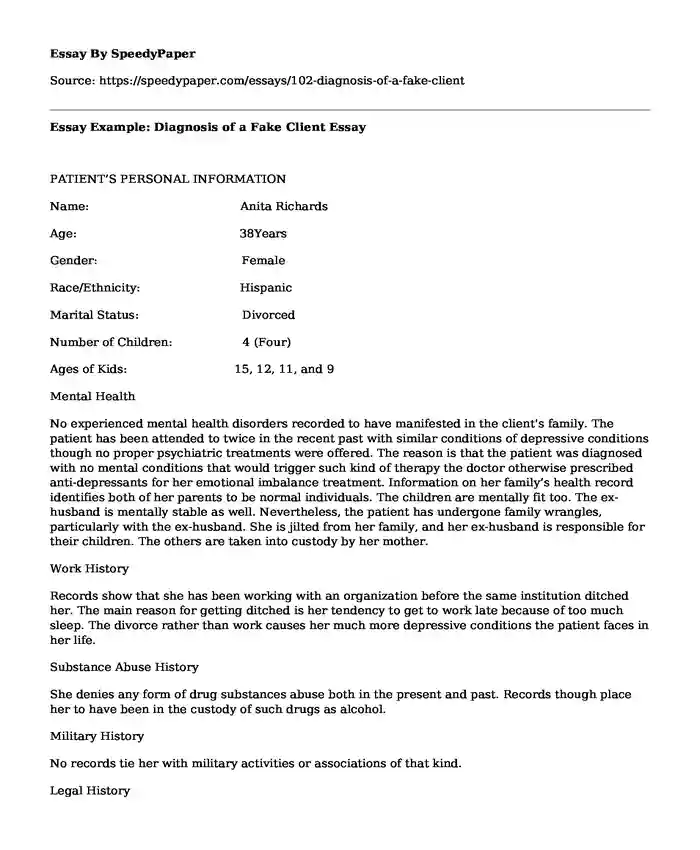
PATIENT’S PERSONAL INFORMATION
Name: Anita Richards
Age: 38Years
Gender: Female
Race/Ethnicity: Hispanic
Marital Status: Divorced
Number of Children: 4 (Four)
Ages of Kids: 15, 12, 11, and 9
Mental Health
No experienced mental health disorders recorded to have manifested in the client's family. The patient has been attended to twice in the recent past with similar conditions of depressive conditions though no proper psychiatric treatments were offered. The reason is that the patient was diagnosed with no mental conditions that would trigger such kind of therapy the doctor otherwise prescribed anti-depressants for her emotional imbalance treatment. Information on her family’s health record identifies both of her parents to be normal individuals. The children are mentally fit too. The ex-husband is mentally stable as well. Nevertheless, the patient has undergone family wrangles, particularly with the ex-husband. She is jilted from her family, and her ex-husband is responsible for their children. The others are taken into custody by her mother.
Work History
Records show that she has been working with an organization before the same institution ditched her. The main reason for getting ditched is her tendency to get to work late because of too much sleep. The divorce rather than work causes her much more depressive conditions the patient faces in her life.
Substance Abuse History
She denies any form of drug substances abuse both in the present and past. Records though place her to have been in the custody of such drugs as alcohol.
Military History
No records tie her with military activities or associations of that kind.
Legal History
Records, though, provide situations of being jailed for possession of drug substances. The patient explains that the reason for ownership includes making a living out of the activity but not rather consuming the substances.
PATIENT’S PRESENTING PROBLEM
The patient is majorly suffering from emotional conditions. She presents herself in the facility unkempt and shaggy. Her eyes appear puffy and a bit swollen. The client records being jilted from her working premises and also not being able to get any other job later after being fired from work. Another presented problem which is part of her health condition is the inability to take care of her children. After breaking up with her ex-husband, she reports having unceasing crying jigs which majorly contributes to the deterioration of her health. Because of the extremely stressful conditions presented by the patient, she does not feel any sense of security and therefore views herself as extraordinarily useless. The feeling makes her dangerous to herself. Some of the risk factors contributing to her conditions include being neglected by her immediate family, sexual uncertainties or possible verbal abuses and lastly, uncertain environment.
The conditions manifesting in the client leading to the conclusions stated earlier in this section include:
i) Terrible occurrences of mood swings
ii) Consistent self-blame and subject to guilt
iii) Feeling of absolute hopelessness and extreme sadness
iv) Irresistible fear and state of anxiety
v) Feeling of being disconnected and general numbness
vi) General fatigue and getting startled
vii) A lot of muscle tension and aches
viii) The inability to concentrate
ix) Getting withdrawn from others
DIAGNOSTIC IMPRESSIONS
Major Depressive Disorder (MDD) Therapy and Treatments
According to the underlying conditions, the patient is recommended to undergo a MDD treatment. The main reason for choosing this treatment regime is to alleviate the manifesting situation of the Major Depressive Disorder. Because the patient happens to be experiencing severe forms of anxiety disorders, MDD therapy is convenient. Cognitive Behavioral Therapy (CBD) will help in recognition of thought patterns of the patient and ascertain if the patterns of behavior of the patient are faulty and deserve addressing. Since the patient is recording an incorrect assessment of danger following her situations and passing self-threat, it is wise to induce CBT for MDD instead of other methods of PTSD-like hypnosis and art therapy.
CULTURAL CONSIDERATIONS
Consequently, other forms of mental illnesses like panic disorder and the bipolar disorder have the same recognizable conditions in almost all parts of the world. Culture, therefore, influences how a patient may describe his mental condition to a physician. The patient reports facing emotional symptoms as a physical condition. Cultures always vary particularly when the word is used in the description of an illness or the impact a condition has on a patient. The meaning of the word ought to be deep-seated and portray whether the disease is real or just imagined. In this case, the descriptions provided by the patient are as a result of the state of mind. Culture will, therefore, play an important role in motivating the patient to adjust to the treatment regime. The parents of the patient and the individuals close to her must realize that they are the determinant of the rate at which the patient responds to treatment or not. In this case, the parents and the ex-husband must be involved in her treatment schedule.
HEALTH CONDITIONS
The patient is diagnosed with a severe form of emotional conditions. The condition is prevalent and therefore the treatment regime recognized to produce impact include:
i) Administering Depressive Therapy and treatment
ii) Administering Electroconvulsive Therapy and Reprocessing Medication
iii) Administering Light Therapy
CLINICAL IMPRESSIONS AND PROGNOSIS
In this case, the screening processes used in determining the amount of mental breakdown of the patient produced positive results. Most of the factors used to conclude depressive devastation were coinciding with the patient's responses. However, the client possesses no such symptoms warranting severe psychiatric treatment interventions. The patient's history provides evidence that she faced MDD in her life before. The assessment made gathers all the information relating to the methodology of understanding the impact of the conditions on the life of the patient. The overall evaluation entails:
i) Performances of major blood and urine tests to rule out other possible conditions.
ii) The patient thinks she is utterly useless and thus has no value in life.
It is speculated that one may start feeling fine in just few weeks of continuous treatment. The patient will still need to be on medication for quite a long time in order to feel completely well and mitigate the symptoms of depression from returning. In case of conditions of chronic depression, other forms of illnesses like heart diseases and diabetes can’t be easily managed. The patient is also advised to avoid consuming drugs that are harmful to the body system.
TREATMENT PLAN
Treatment involves administration if drugs and also conducting therapeutic talks. In this case, the patient will be treated using anti depressants. The functions of the drugs include making sure that the chemical properties of the brain are dropped to the normal level of functionality. In case of delusions, additional drugs are prescribed for the patient. The drugs to be prescribed include:
i) Selective Serotonin Reuptake Inhibitors (SSRI)
These kinds of medication are thought to be safer and cause fewer side effects. They include Prozac, Pexeva, Zoloft, Celexa and Lexapro.
ii) Serotonin-norepinephrine Reuptake Inhibitors (SNRI)
Examples include Cymbalta, Effexor XR, Khadelza and Fetzima.
iii) Norepinephrine-dopamine Reuptake Inhibitors (NDRI)
Under this category are drugs such as the Bupropion. It is an antidepressant and advantageously not associated with any form of sexual side effects.
iv) Atypical Antidepressants
Under this category, examples include Trazodone and Remeron.
v) Tricyclic Antidepressants
These drugs happen to be very effective and are thus prescribed where other drugs aren’t effective in curing. They include Trofanil, Pamelor, Surmontil and Vivactil.
vi) Monoamine Oxidase Inhibitors
These drugs thoroughly interact with foods such as cheese and wine and also other forms of medication including birth control pills, herbal supplements and decongestants. Patients are therefore advised to undertake a strict diet. The MOIs can’t therefore be associated with SSRIs.
Other medications can also be used alongside the listed ones to increase the effectiveness of the drugs and to produce the required outcome. The doctor may prescribe a combination of two or more antidepressants to stimulate quick drug response towards the condition.
Reference
Chadwick, O., Rutter, M., Brown, G., Shaffer, D., & Traub, M. (1981). A prospective study of children with head injuries: II. Cognitive sequelae | depressive medicine | Cambridge core. Depressive Medicine, 11(1), 49–61. doi:10.1017/S0033291700053277
Staff, M. C. (2016). Depression (major depressive disorder) treatments and drugs. Mayoclinic. Retrieved from http://www.mayoclinic.org/diseases-conditions/depression/basics/treatment/con-20032977
Major depression. (2017, February 7). Retrieved February 12, 2017, from https://medlineplus.gov/ency/article/000945.htm
Cite this page
Essay Example: Diagnosis of a Fake Client. (2018, Feb 27). Retrieved from https://speedypaper.com/essays/102-diagnosis-of-a-fake-client
Request Removal
If you are the original author of this essay and no longer wish to have it published on the SpeedyPaper website, please click below to request its removal:
- Minimum Wage - Economics Essay Example
- Free Essay Sample on Courage and Calling
- Free Essay: Book of Romans Chapter One Analysis
- Free Essay: The Experiences of Female Students With Sexual Abuse in School
- Articles Analysis Essay Sample on Obesity
- A Doll's House: Literary Analysis
- Free Essay - Stetler's Model of Research Utilization
Popular categories




