| Type of paper: | Essay |
| Categories: | Health and Social Care Medicine |
| Pages: | 4 |
| Wordcount: | 1037 words |
Chronic obstructive pulmonary disease (COPD) is an ailment that is described by the limitation of airflow to the lungs; although this disease is typically dynamic, not completely reversible and connected to an inflammatory reaction of the lungs one can be treated and prevented from it. COPD is majorly attributed to introduction of noxious substances to the lungs, mostly caused by cigarette smoking though other factors may bring about such a condition. It is used to describe two lung related diseases namely; chronic bronchitis and emphysema. Chronic bronchitis is defined clinically as a chronic steady cough for 3 continuous months every year for 2 sequential years in which the side effects worsens. Emphysema is the lasting and anomalous broadening of any part of the air spaces distal to the terminal bronchioles. Emphysema likewise includes annihilation of the alveolar walls without fibrosis. The COPD excludes other obstructive lung sicknesses, for example, asthma, despite the fact that asthma has the same pathophysiologic shared factor as chronic bronchitis also, emphysema, which slows down the breathing rate (Buttaro, 2013).
COPD Diagnosis
Early location of COPD is imperative for diminishing the related dreariness and mortality. Side effects of COPD don't for the most part happen until a lot of lung harm has happened. Some of the clinical diagnoses considered are; a straightforward office move called forced expiratory time may figure out whether further testing is required and should be confirmed by spirometer since it is the most reproducible, institutionalized, and target method for measuring airflow limitation.
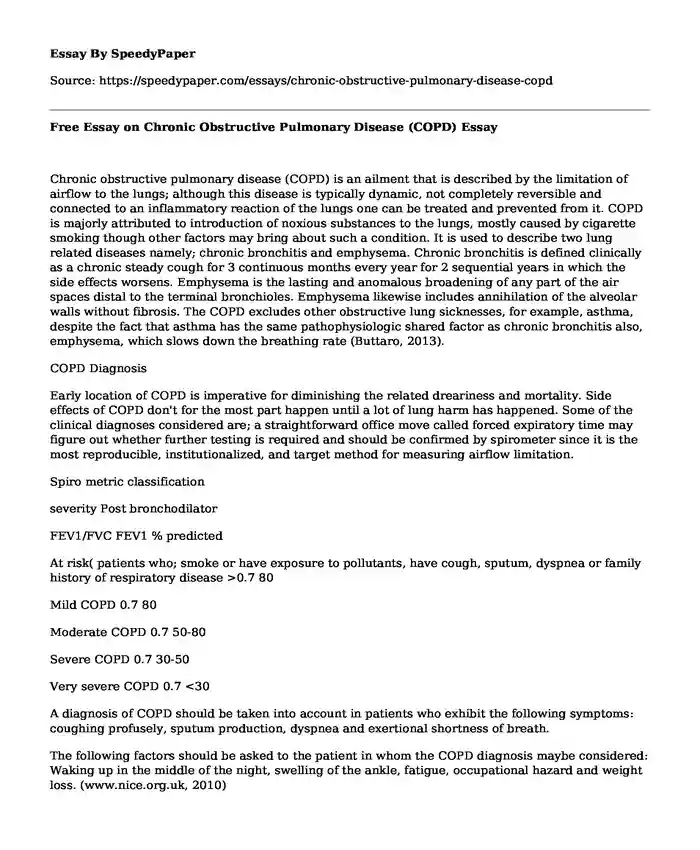
Spiro metric classification
severity Post bronchodilator
FEV1/FVC FEV1 % predicted
At risk( patients who; smoke or have exposure to pollutants, have cough, sputum, dyspnea or family history of respiratory disease >0.7 80
Mild COPD 0.7 80
Moderate COPD 0.7 50-80
Severe COPD 0.7 30-50
Very severe COPD 0.7 <30
A diagnosis of COPD should be taken into account in patients who exhibit the following symptoms: coughing profusely, sputum production, dyspnea and exertional shortness of breath.
The following factors should be asked to the patient in whom the COPD diagnosis maybe considered: Waking up in the middle of the night, swelling of the ankle, fatigue, occupational hazard and weight loss. (www.nice.org.uk, 2010)
COPD Management
There are two ways in which a patient diagnosed with COPD can manage their conditions; they can achieve this through pharmacological and non-pharmacological interventions. Non-pharmacological interventions include: smoking cessation where the patient reduces the risks associated with smoking, encouragement of physical exercises, nutritional review, educate patients on avoidance of aggravating factors. Pharmacological interventions include: oxygen therapy, immunization against respiratory pathogens, there are surgeries that may assist some patients namely lung volume reduction surgery (LVRS) and lung transplantation and lastly administration of drugs that may assist to improve lung function though cannot offer any treatment. (www.thoracic.org, 2004)
COPD prevention strategies
The best way to prevent the accelerated cases of COPD would be to educate the community on OCPD prevention measures to ensure they live a healthy lifestyle. The public should know what are the major causes of OCPD and how to avoid them, for those who are already affected learn how to contain it because it is a progressive disease.
COPD case study
On 24th of March 2016 from 8-9pm met with a patient named John. John, a 68 year-old male, has been feeling unwell throughout the previous 5 days, and feels 'winded' and wheezing more. He couldn't walk more remote than 5m, from his seat to the latrine. He has an intensifying cough and has been creating yellow/green sputum. He calls his GP surgery in the morning, and tells the assistant of his side effects, and is booked a meeting with his GP, later that evening. His significant other goes with him and says he has turned out to be excessively short of breath, now and again, making it impossible to try and talk or eat. The patient feels entirely befuddled and disorientated.
PMH: COPD, Type 2 Diabetes (controlled by diet only), conceded a month back with mid-section contamination.
Tallness: 70 kg, 175cm
Current Medication:
Salbutamol 100 micrograms MDI, 2 puffs when required up to 4 times everyday.
Clenil Modulite (Beclometasone dipropionate) 100mcg MDI CFC- inhaler: 2 puffs two times a day with spacer gadget.
Social Habits: Heavy smoker smoking 20 cigarettes/day since 14 years of age (54 pack-years). Right now lives in 3-room house alongside his significant other. As of late resigned 8 years ago as a processing plant vendor. Surrendered liquor around 5 years ago.
Sensitivities: nil & NKDA.
He underwent spirometry, some weeks ago and the outcome showed:
FEV1: 1.56L (Predicted FEV1: 3.07L)
FVC: 2.28L
FEV1/FVC: 0.68 (68%)
51% of Predicted FEV1 normal
His GP, Dr Kingston alluded him to the clinic, and he is admitted to the Respiratory Ward, by means of A&E. Examination uncovered diminished breath sounds, across the board expiratory wheeze and summed up hyper-reverberation. He was halfway cyanosed, and his SpO2 levels were between 84 - 85%.( Dodds,2010)
Patient diagnosis
John has been receiving treatment as an asthmatic patient
The treatment for COPD is quite different from asthma
To manage his COPD current therapy must be reviewed
Optimize therapy:
- Beclometasone dipropionate without CFC or any ICS - not authorized for patients with COPD (unless recommended in mix. with a LABA) yet assists with the intensifications.
- Bronchodilators might be underused if individuals with COPD are overseen as asthmatics. In symptomatic patients the foundation of administration of shortness of breath in COPD is breathed in bronchodilation. In spite of the fact that they don't fundamentally enhance lung capacity (FEV1), bronchodilators enhance shortness of breath, activity limit Short-acting bronchodilators, for example, salbutamol, terbutaline or ipratropium are given for alleviation of discontinuous windedness and can be utilized routinely for the duration of the day, regularly at higher than authorized dosages.
Start antibiotics and steroids
Monitor blood glucose thro BM Stix and the respiratory rate of the patient
References
Buttaro, T. (2013). Primary care. St. Louis, Mo.: Elsevier/Mosby.
Chronic obstructive pulmonary disease in over 16s: diagnosis and management. 1-guidance. Guidance and guidelines | NICE. (2010). Nice.org.uk. Retrieved 9 June 2016, from https://www.nice.org.uk/guidance/cg101/chapter/1-Guidance
American Thoracic Society - COPD Guidelines (2004). (2016). Thoracic.org. Retrieved 9 June 2016, from http://www.thoracic.org/copd-guidelines/
Lung Foundation Australia. (2016). Lungfoundation.com.au. Retrieved 9 June 2016, from http://lungfoundation.com.au/Dodds, L. (2010). Drugs in use. London: Pharmaceutical Press.
Cite this page
Free Essay on Chronic Obstructive Pulmonary Disease (COPD). (2019, Sep 30). Retrieved from https://speedypaper.com/essays/chronic-obstructive-pulmonary-disease-copd
Request Removal
If you are the original author of this essay and no longer wish to have it published on the SpeedyPaper website, please click below to request its removal:
- Arguments for and Against the concept of Peak Oil. Free Essay on Energy.
- Asking Mr. Bill for an A, an Argumentative Essay Sample
- Free Essay: An Analysis of the Marketing and Public Relations Sectors
- Employee Engagement - Free Essay Example
- Free Essay Investigating the Effects of Social Media on Adolescents and Young Adults
- Exploring Hydroxychloroquine: Uses, Controversies, and Ethical Concerns in the COVID-19 Era - Free Essay
- Maternal and Child Health - Essay Sample
Popular categories




